Vitiligo Condition
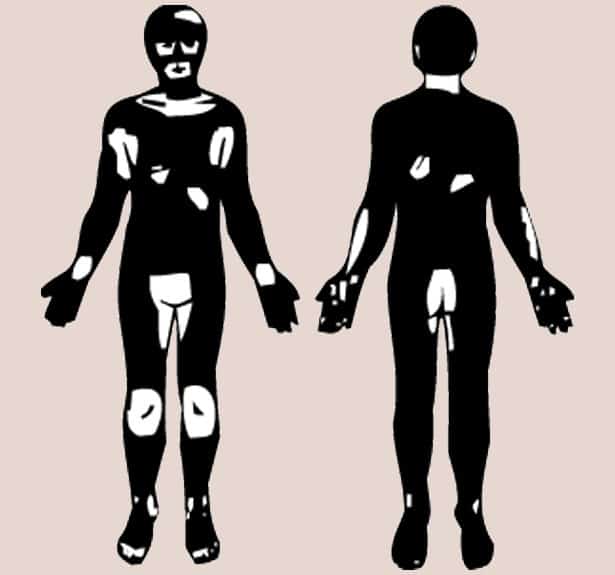
Vitiligo is a condition in which your skin loses melanin, the pigment that determines the color of your skin, hair and eyes. If the cells that produce melanin die or no longer form melanin, slowly growing white patches of irregular shapes appear on your skin.
Vitiligo Usually
Vitiligo usually starts as small areas of pigment loss that spread and become larger with time. These changes in your skin can result in stress and worries about your appearance. There is no cure for vitiligo. The goal of treatment is to stop or slow the progression of depigmentation and, if you desire, attempt to return some color to your skin.
Vitiligo Skin
Vitiligo: (vit·i·li·go) Vitiligo is a skin condition of white patches resulting from loss of pigment. Any part of the body may be affected. Melanin, the pigment that determines color of skin, hair, and eyes, is produced in cells called melanocytes. If these cells die or cannot form melanin, the skin becomes lighter or completely white. Affected skin is particularly sensitive to sunlight.